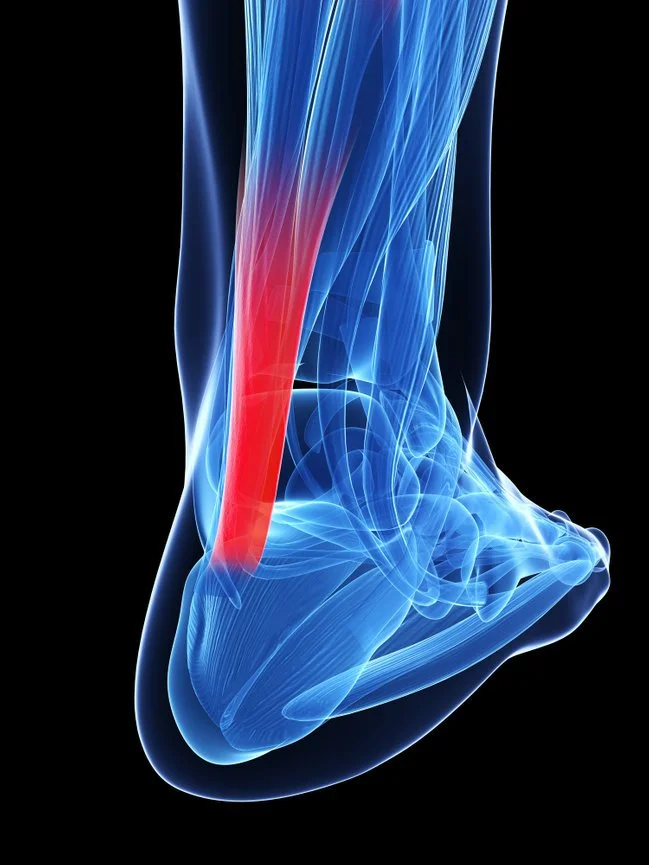
Achilles Tendonitis
Achilles tendinitis (or tendonitis) is the inflammation of the Achilles tendon, the strong band of tissue that connects your calf muscles to your heel bone. This tendon is used every time you walk, run, jump, or stand on your toes, making it one of the most commonly injured tendons in the body.
-
Achilles tendinitis often develops due to repetitive stress or overuse. Contributing factors include:
Intense or sudden increase in physical activity
Tight calf muscles
Bone spurs (extra bone growth at the heel)
Improper footwear
Rheumatoid arthritis or infection
Degeneration of the tendon over time
-
Stiffness or pain along the tendon, especially in the morning
Swelling or thickening of the tendon
Heel pain that worsens with activity
Tight, stiff calf muscles
Warmth or tenderness at the back of the heel
Limited ankle flexibility
-
Insertional Achilles Tendinitis – inflammation where the tendon attaches to the heel bone, often associated with bone spurs.
Non-Insertional Achilles Tendinitis – degeneration, swelling, and tiny tears in the middle portion of the tendon, more common in younger, active people.
-
Untreated Achilles tendinitis can progress to:
Severe, chronic pain
Difficulty walking or exercising
Deformity of the tendon or heel bone
Complete tendon rupture requiring surgery
-
1. Try This at Home
RICE protocol – Rest, Ice, Compression, and Elevation
Supportive shoes and activity modification
Over-the-counter NSAIDs for pain and swelling
2. Podiatrist-Guided Care
Custom orthotics or braces to offload the tendon
Physical therapy with stretching and strengthening exercises
Shockwave Therapy (ESWT) – non-invasive, high-energy sound waves that stimulate healing of chronic Achilles tendon injuries and reduce pain without injections or surgery
Ultrasound-guided injections – PRP (platelet-rich plasma) to reduce inflammation and promote tendon healing
3. Surgical Treatment (if conservative care fails)
If symptoms persist after 6 months, surgery may be recommended. Options include:
Debridement and repair – removing damaged tissue and repairing the tendon
Debridement with tendon transfer – if more than 50% of the tendon is damaged, tissue from another tendon may be used to strengthen it
Gastrocnemius recession – surgical lengthening of calf muscles for patients with limited flexibility
Open repair or minimally invasive repair for complete ruptures
Disclaimer: The information on this website is for educational purposes only and should not replace professional medical advice, diagnosis, or treatment. Always consult your doctor with any questions about your health.